We got a look at a new report today. The hospital is all about hiring consultants and then systemically ignoring what they tell us. Our latest visit was from Dr. Ragins of MHA-LA.
I suspected we would never see a non-redacted version of his recommendations but I’ve been proven wrong.
Here it is, along with a older report he did as a pdf link. I’ve also included the introductory letter from our CMO, Dr. Rupert Goetz.
December 6, 2013
To: All affected staff
From: Rupert Goetz, MD
Subject: Attached Consultative Report
As we move into this biennium, one of the changes we are pursuing is to strengthen our understanding of “Recovery” at OSH. Hope, Safety and Recovery are after all the three core concepts in our Vision Statement.
In strengthening our understanding, we want to build on our past (remember the collaboration between Dean Brooks and Maxwell Jones around the Therapeutic Community concept; remember more recently the visit by Sandra Bloom around the Sanctuary Model). But primarily, we want to look forward. We want to look at the many ways we can grow together. For example, we also want to better understand how peer-delivered services can help us build our desired culture.
To that end, I asked Mark Ragins, M.D., who has for years helped implement the recovery model at The Village in California, to visit with us and share his thoughts. Attached is his report.
The purpose of the visit and of sharing the report is to provide us with an outside perspective. While we want to honor our past, as well as our many current internal champions, we want to creatively plan our path forward together. This additional perspective is intended to help us do so.
There are minor details such as the “not guilty” reference (it is in Oregon “guilty except for insanity”) that we might want to quibble with. There may also be the assumption that this is the blueprint for our work in the coming year – it is not. I hope rather that you find it a thought-provoking place to begin our conversation about how we strengthen recovery at OSH.
Oregon State Hospital Recovery Transformation Consultation Report
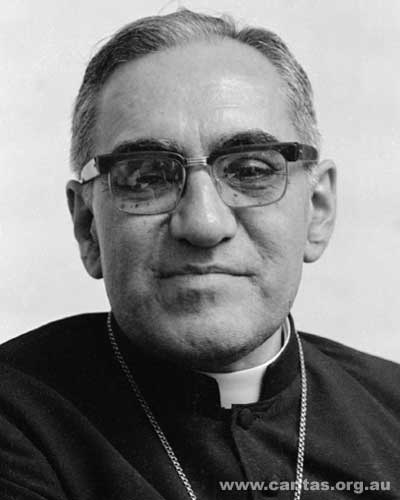
Mark Ragins, MD
Acknowledgements:
I want to thank the Oregon State Hospital for welcoming me to share your work and your lives with me. A friend of mine defines welcoming as “opening a space in your life for a guest to feel comfortable and opening yourself up to them, knowing full well your guest may change you in unexpected ways.” I have felt truly welcomed by you. I hope I have been a good guest.
This report is not meant to be an expert, authoritative evaluation and orders for you. Recovery transformation is a complex problem and complex problems are not solved by outsiders or by definitive answers. Successful transformation is an evolving, collaborative process that never ends. At best my influence can by to support, nurture, inspire, instruct, guide, and share your organic process of growth. The explorations, observations, thoughts, and suggestions I’m writing here are just the current iteration of my evolving reactions.
I have attached a large volume of reference material from our work at MHALA and the Village. These are not meant to be blueprints for you to replicate the Village or even an instruction book for you to build your own program. They are concrete, real world, useful tools we have evolved in our own process that may inspire your imagination of what possibilities you might pursue. Remember that they have evolved over decades of work at MHALA and the Village…and we’re not slow learners; we’re aggressive innovators.
A note on language in this report: The words I most commonly heard you use to describe the people you serve were patient and client. There was widespread distaste for the word inmate. In other places I’ve seen people also called residents, guests, members, students, consumers, people in recovery, etc. It’s likely that each of those words would be an accurate description of roles people have experienced along the way. There is a considerable power in the words we choose and how they reflect our mission and values. Your choice has evolved and may evolve further. I will use patient and client interchangeably in this report to “meet you where you are”.
Recovery and the Oregon State Hospital:
For me the initial overriding question for this consultation was “Is it possible to use recovery as an overarching philosophy and approach at a place like OSH?” Recovery emphasizes concepts like empowerment, self determination, self responsibility, and community integration. The patients at OSH have been specifically selected for people who are unsafe, untrustworthy, incompetent to be held self
responsible, and who have been forcibly excluded from community life. Even for a true believer in recovery and strong advocate like me that seems a difficult challenge.
Can people at OSH actually recover? Over my few days at OSH I saw several things that impressed me that the answer is yes. Firstly, the enormous majority of people at OSH will be living free from restriction in our community at some point in the future. Their day-to-day reality at OSH emphasizes risk assessment, confinement and restriction. But if we take the long view, the vast majority of people realistically should be preparing for freedom, not ongoing confinement. Second, the long term staff I met were all hopeful for the clients they’re working with. They believe things will get better for them. Third, and probably most importantly, there were widespread examples of patients at all points in their journey who are making progress and recovering. These ranged from someone who was soothing himself with a guitar to reduce his assaultiveness and seclusion from every day to a few times a week to a young man doing Calculus homework for his online college class who has been approved for discharge to a group home hoping to continue his studies on campus. Whether you describe yourselves in recovery terms or not, recovery is happening at OSH now.
For recovery to be a pervasive culture, the wide range of hopes, dreams, and personal journeys of each patient’s recovery need to be unified into a shared collaborative vision and destination. My proposal is: People living at OSH are engaged in a hopeful, healing journey towards freedom, safety, and self responsibility. I believe that those three characteristics of the destination – freedom, safety, and self responsibility – are all mutually interdependent. None can be sustained independently without the other two. Whichever of the three are not addressed and achieved will ultimately drag down the other two. I believe that vision of recovery can be applied throughout OSH.
My next concern about implementing recovery was “Is it possible for the staff to have relationships with the clients that regularly support and facilitate their recovery?”
The clients at OSH are in a strange, awkward moral place where society has rejected them without convicting them of any crime. The staff must be “abnormal in a certain special way” in order to reach out supportively to people who have been cut off and exiled by our society. To create a “counterculture of acceptance” at OSH staff must be consistently accepting of them. It seems as though the majority of your staff is already there.
It would be helpful to have a unifying “moral stance” regarding the clients that everyone accepts. I would propose: These people have been determined not to be guilty, bad people who should be punished, but rather incapable people who should be supported to become capable again. This stance is consistent with the recovery vision above. Staff who become punitive instead would need to be sanctioned. It would also be helpful to include the ability to accept your clients on that basis as part of your recruitment, hiring, orientation, training, and retention.
The other serious obstacle to forming recovery relationships is the danger staff are in because of the patients’ violence and the fear the staff feel as a result. It is extremely difficult to collaborate with and empower someone we’re frightened of. A good deal of the staff seem to have embraced trauma
informed care as a tool for reducing fear, conflict, power struggles, and actual danger. This should become universal.
Beyond that, the most impressive thing I saw at OSH was the innovative and exemplary practice on a very dangerous unit: They have come together as an amazingly unified team, using a detailed, highly individualized “engagement” tool that assesses each person’s dangerous behaviors including their triggers, warning signs, helpful relationships, self soothing and care combined with a DBT approach. The staff never give up and continue to seek out creative approaches for each person gaining administrative approval when exceptions to policy need to be made. They appear to have drastically reduced the dangerousness on the ward. Beyond that, even though there continue to be assaults and seclusion and restraints, the staff feel safe and are allied with the clients. This is a remarkable accomplishment that should be analyzed, replicated, rewarded, and treasured. I believe that if it can be done widely alongside trauma informed care, it can get you through the fear barrier to recovery relationships.
I think more work could be done proactively and on an ongoing basis to keep staff from becoming too fearful and traumatized. Your staff have to have the resilience to feel safe even though they’ve been assaulted and likely will again. They may need to be selected for that trait (from a variety of experiences). They need support when they’re weakened and need recharging. They need each other most of all. Toughing it out alone or feeling trapped with a certain patient or unit are both likely to lead to burnout. Ongoing attention to staff nurturance to avoid fearfulness is essential.
My conclusion is that – with ongoing support and emphasis – enough hope, acceptance, alongside enough avoidance of fearfulness and punitiveness could be maintained to have recovery relationships throughout OSH.
What advantages would recovery likely have at OSH that would make it worth the effort?
- Integration of services: There is a dazzling array of services at OSH ranging from psychiatric medications, to external controls, to sex offender therapy, to art and music therapy, to supported employment, to peer advocacy and bridging, to access to a legal library, to discharge resource development, to an Empowerment center, to yoga and mindfulness, to anger management and substance abuse groups, to Basketball and a woodwork workshop, etc. Although there are some team meetings and a coordination plan much of what is done is not integrated together. A recovery focus brings the utility of each activity into focus: Does this activity move the person closer to freedom, safety, and self-responsibility from where they are now? There is far less need for power struggles and hierarchies to determine whose work gets priority if you’re all in alliance working on the same goals in the same direction. It would also be clearer to the patient how everything fits together to benefit them.
- Decreasing “staff vs. patient” conflicts: Recovery emphasizes collaboration, shared decision making, and empowerment rather than compliance, informed consent, and professional authority. Those differences radically reduce conflict. Safety would likely be improved for both staff and patients as a result.
- Decreased staff burnout and increased satisfaction: One of the most powerful factors behind the spread of recovery is how much staff prefer it once they are doing it openly and together and confidently compared to their previous work. At bottom, recovery feeds our hearts more than standard treatment does.
- Alliance between administration and staff: if administration embraces and adopts recovery practices for themselves in addition to prescribing it for their line staff the entire program works more synergistically.
- Improved community advocacy: When community advocacy is based on fear and “demonizing” our patients we can get extra money, but we badly decrease community welcoming and reintegration for our patients. When community advocacy is based upon recovery, we can ally with our patients, and we have a foundation for promoting community welcoming and reintegration. Telling stories of patients achieving safety, freedom, and self responsibility are far more likely to help them be accepted than billboards of staff injuries at the hands of dangerous, frightening patients.
- Protection against slipping into dehumanized, punitive, coercive relationships: Any program that is involuntary, locked, and largely hidden from society is prone to slip into increasingly dehumanized, punitive, relationships and from there into overt abuse. Power is corrupting. A recovery culture can provide a counterinfluence to these destructive trends.
Recovery implementation:
Recovery is primarily a treatment culture. It emphasizes less what is done and more how and why it is done. Therefore, implementing recovery is a prolonged, organically evolving, complex process. It needs to be tended and nurtured like a farmer does, not blueprinted and built like an engineer does. Take your time. Be gentle to the land and be a good farmer: Till the soil to prepare it, help pick out seeds and pay for them, plant alongside the staff and clients, fertilize and nurture seedlings, pull out weeds (but not with widespread poisons), rotate crops to avoid exhaustion, and celebrate the harvests together.
There are many recovery principles and practices – like “client-driven” or managing relationships during times of transition to promote growth and self responsibility or strengths based community advocacy – that require years to explore and master. Be patient. Here’s a link to something I wrote to comfort and guide transformational leaders: http://mhavillage.squarespace.com/storage/69KeepingPerspectiveandStayingSane.pdf.
The land can be plowed by mapping recovery. There are a number of “maps” of recovery to adopt from, but you should create your own and it should be very specific to your clients’ journeys. Years ago I created a four stage “map” for the Village based on the work of Elizabeth Kubler-Ross that includes four stages– hope, empowerment, self-responsibility, and achieving meaningful roles. http://mhavillage.squarespace.com/storage/08ARoadtoRecovery.pdf is a link to my short book “A Road to Recovery” that describes this map using lots of stories and learning from our direct experiences at the Village.
Your map could include stages like:
- Being involved in a tragic, socially forbidden action,
- being determined to be incapable of self responsibility and punishment and referred to OSH to rebuild capability,
- being faced with unwanted external control and coercion,
- being stuck in resentment and rebellion,
- resisting change and trying to “fake it to evade it”,
- feeling ongoing pressure for internal change,
- demoralization and giving up,
- maladaptation to living in the institution,
- having seeds of trust and collaboration with staff to try to rebuild,
- prolonged internal self-evaluation and skill building in a variety of ways,
- repeated cycles of failing to do enough to be released,
- achieving release status but no community opportunities or resources,
- being released and facing ongoing coercion and control and community rejection,
- returning to unsafe behaviors and environments,
- achieving full freedom, safety, and self responsibility.
It is essential that this map be from the clients’ point of view to be a recovery map. (If it’s from the staff’s point of view it’s a treatment map, not a recovery map.) The “gold standard” is that the clients can recognize themselves and their journeys on the map. Make every effort to amplify the clients’ voice and experience. Embellish the map with client stories, artwork, music, video, poetry, etc. Here’s a link to a touching example of a video created by a group of consumers in Porterville, California: http://www.youtube.com/watch?v=uH9gV_7jmiQs.
You can gain some cultural depth by connecting the map to other human journeys (like achieving death with dignity, Joseph Campbell’s hero’s journey, 12 step journeys, or other recovery narratives, etc.)
You can also gain some spread of this map from just applying to clients to applying to everyone by creating a narrative of the recovery process OSH has experienced going through the same stages as the clients. It almost seems uncanny to me how closely these stages describe the last few years at OSH. MHALA applied the same four stages our members go through to what staff go through when we structured our Recovery Oriented Supervision trainings to emphasize that we need to treat our staff the way we want them to treat our clients.
Your recovery map can then be a direct guide for determining how staff relationships facilitate or hinder recovery at each stage, how services should be organized and integrated “meeting clients where they are at”. A standard for valuing staff and services becomes “How does this promote your client’s recovery?” rather than which staff has more power or influence within the system or hierarchy. This also makes the resolution more often “and” rather than “or” valuing each staff and service for their strengths and figuring out how they can work together instead of competing against each other. (For example, a team with a united front demonstrating a “show of force” standing behind an individual staff with a soothing relationship trying to help an aggressive client problem solve and re-establish self
control can work together without either one being “wrong”.) It should be possible to promote efforts that strengthen people without weakening someone else.
The Village found that our treatment principles mapped directly onto our four stages map too (see attachment 1). Notice how precisely stated and focused our principles are. You may have staff that are good at developing clear treatment principles that apply across OSH defining the “beliefs” that underlie your evolving recovery culture.
Administratively, you want to develop parameters to guide staff as they develop individualized recovery relationships rather than highly prescriptive policies, especially avoiding pervasive “thou shalt not” policies that “straightjacket” them. This link has a set of parameters that the LA County Department of Mental Health developed and adopted with our assistance: http://mhavillage.squarespace.com/storage/82NewRulesforStafftoWorkBy.pdf.
OSH staff expressed a lot of change fatigue and burnout. My overall impression is that there are more people who think there have been too many changes, especially administratively engineered changes, than people who think that OSH is stagnant at present. Top down engineered changes engender more change fatigue and resistance than bottom up, organically emerging changes. Except for three pointed exceptions I’ll describe below, I would recommend cultivating currently emerging changes instead of directing new mandates. (For example, after I visited a state hospital in Provo, Utah each staff member made a large cutout of a helping hand with one thing they would do differently to support hope, empowerment, self responsibility, or meaningful roles and then the patients responded by each of them making a large cutout of a foot with one thing they would do to walk a path with more hope, empowerment, self responsibility, and meaningful roles. A lot of excitement and empowerment was generated there by this approach.)
Promising examples of emerging changes I heard about at OSH included:
- Trauma informed approaches to reducing seclusion and restraint and increasing self control
- Team based integrated engagement and DBT approaches to reducing aggression and assault
- Creating more “nimble teams” that could rapidly solidify trust even with staff movement and turnover
- Enhancing peer support services
- Specialized ethnic and sexual orientation specific peer support
- Using music recording to explore personal growth and create positive roles
- Using yoga to address trauma wounds and healing in non-verbal ways
- Create a robust family and community volunteer presence in the treatment malls to increase community connections and acceptance
- Create a client key card system so that increase privileges and self responsibility are directly connected with increased freedom of movement around OSH. (BTW I saw this done successfully in that same state hospital in Provo Utah)
- Openly discuss and develop parameters for including positive, permissible sexual activities including dating, hugging, dancing together, and conjugal visits.
- Increase peer bridging to peer run organizations n the community to increase community supports and connections upon initial release from OSH
- Creating a newsletter with stories of hope and recovery
I’m sure there are many more seeds and saplings of ideas around that need nurturance.
Hope requires a lot of consistent nurturance built into your program or we end up focusing on the crises of the day and the things that go wrong. ( Examples of hopeful rituals include beginning team meetings with stories of hope, regular celebrations, special staff acknowledgments and rewards, etc.) Too many policies are made to make sure one serious incident “never happens again” instead of strengthening us so when something tragic happens, and it inevitably will, we’re able to continue on.
The three area in which I would recommend you do serious course corrections (or to use our sailing metaphor, three places where I think you should tack – including communicating the need for a course change, micromanagement of the course change, and bringing people together to handle the change as a team) are: 1) personal dedicated recovery relationships, 2) peer support services, and 3) board hearings.
1) Personal dedicated recovery relationships:
Your present system tries to ensure that everything is in place to facilitate someone’s recovery. They have written goals and a recovery treatment plan. They have the availability of a wide variety of supports and services which they are scheduled into. And they have clear objective assessments to prepare them for hearings and release. What they don’t always have is a trusting, collaborative relationship with a single dedicated staff to guide them through the process. This staff also needs to guide them through the internal process of recovery – engagement, motivational enhancement, commitment, dealing with grief and loss, internalizing skill building and role changes, moral development, building self responsibility and self reliance, preparing for discharge and community belonging.
I strongly prefer a “therapist case manager” model to a “broker case management” model for this primary relationship so that the internal and external processes of recovery can be integrated. At the Village we call this person a “Personal Service Coordinator” and have adopted Kansas University’s “strengths based case management” model.
I fear that implementing a PSC model at OSH will require substantial top-down structural reorganization, precisely of the kind resented by your staff and causing change fatigue and burnout. Nonetheless, I think it’s a crucial course correction.
This is an opportunity to emphasize some of the more personal aspects of recovery relationships instead of making administrative assignments: Which staff is the best personal fit for this patient? Who has the most hope? Who has the least fear? Who has personal life experiences that enable them to connect to this person and inspire them? Who is strongest at the particular phase of recovery this person is in?
Client empowerment can also be overtly included: Who do you want to work with? Who do you trust
the most? The Village even has “open enrollment” periods every six months when our members can switch PSCs or teams within the same level of care without needing to give a justification.
2) Peer support services:
There comes a point in the development of peer services when they need to move from being “angry outsider advocates” to “collaborative, insider reformers” to move forwards. As the walls keeping the patients’ voice silenced are lowered, other voices besides aggressive, antagonistic, self righteous voices can be heard. This is a disorienting time for peer advocates. The traits that have been absolutely essential to lowering those walls and bringing about change, that have been nothing less than heroic, are now being criticized and blamed for not being able to progress further. Newer peer staff may not respect their contribution and what they’ve been through so they could have a voice. These experienced peer advocates may not even agree that there has been substantial progress or that the walls have been lowered. They may fear a “trick” to weaken them or co-opt them. And sometimes they will be right.
But at other times, when the swords are put down, there is a flourishing of other voices and relationships. Sometimes a Nelson Mandela emerges from the fight instead of dying on the battle field like Che Guevara did. Sometimes unions that were regularly striking and being repressed engage in collective bargaining or even shared ownership.
In my opinion, OSH has made enough progress to try to put the swords down. I would recommend substantially increasing the number of peer staff, while substantially decreasing their adversarial “peer advocacy” in favor of collaborative “peer support” services.
Making that course correction will likely be quite difficult. In my experience in other places what usually happens is that some of the most valued and successful long term peer advocates end up removed or reassigned out of the mainstream to move forwards. That seems a shame to me and I don’t know that it’s the only possible strategy. It does however, open the door for a wider acceptance of, and integration of the other peer supporters with the treatment teams improving the patients’ recovery services directly.
At OSH there is a legal restrictiveness that exists side by side with the clinical services that is very important. This brings up the possibility that some of the most valued, but most dedicated to advocacy, peer staff could be moved into a new robust “peer advocacy” department and separated from the “peer support” department that would become co-supervised by the teams and by peers. I don’t know if that’s been done in other forensic settings. If the peer advocacy service was robust and respected enough it could be a valuable “check and balance” against the corruption of power and coercion that is an ever present risk in involuntary, locked settings.
I would advise having a small team of clients, staff, peers, and administration charged with developing a plan to move to a larger peer staff that is no longer emphasizing advocacy. They should seek out guidance from other exemplary peer services. I’ve been exposed to successful programs at Recovery Innovations, Riverside County and Tulare County in California, and King’s County Hospital in Brooklyn.
NAPS (National Association of Peer Specialists) can probably point you towards further resources. The team would be expected to inform and guide the process of changing course, but the course itself wouldn’t be negotiable.
In my view, the main emphasis at this point in your development is not to accentuate the differences between clients and staff but instead to blur those differences. Justice and righteousness are less crucial than trust and reconciliation. Desegregation, power sharing, collaboration, mutual respect, inclusion, and interdependence would be my points of focus. Towards that end I would hire more “blurred people” – both peer staff who have professional skills and degrees and probably more importantly, professional and para-professional staff that have lived experience of mental illnesses. In addition we need to remember that there are a substantial number of staff who are currently hiding their lived experience out of fear. That is a terrible burden on them and deprives the patients of a considerable source of support and hope. Those staff shouldn’t have to take sides. They should be proud of both their personal and professional gifts and be able to use them without fear.
3) Board hearings:
Although there have been changes in these hearings recently, they are still clearly the cause of major distress, antagonism, hopelessness, and divisiveness. A patient complained that they are arbitrary and unpredictable, often not following the clinical input of the staff, leading him to withdraw and give up in helplessness. A psychiatrist said that he pisses off the public defenders, the district attorneys, and the hearing officers about equally so he must be doing something right. Frankly, that doesn’t’ sound like a collaborative relationship either.
Over the last decade there have been substantial innovations within mental health legal hearings. There are mental health courts and drug courts scattered around where the hearing officer has a personal relationship with the client and actively participates in their recovery: They engage and motivate clients. They grieve and celebrate with clients. They mediate between staff and clients working to improve their collaboration. They actively secure community resources and services for clients. They even hug clients. I am aware of an exemplary court and judge in Nevada County, California who handles the involuntary outpatient commitments (Laura’s Law AOT). The Elyn Saks institute at USC is connected with a large number of resources who could inspire and guide you.
I realize that this recommendation is beyond the scope of my consultation and expertise, but I think these hearings could become a major force promoting recovery – especially as defined by freedom, safety, and self responsibility.
Recovery Accountability:
Recovery sometimes seems so nebulous that it can’t be measured or promoted in an accountable manner. This argument maintains that it’s too non-specific, too subjective, too individualized to quantify or track. Either you have it or you don’t. I don’t agree.
Broadly speaking there are three areas to try to create accountability: 1) Recovery service provision, 2) recovery outcomes, and 3) recovery culture. There will always be a tension between the accuracy and detail of the measurements in the accountability tool and the burden it places on clients and staff. (The Mental Health Center of Denver is very sophisticated in their use of data driven management and accountability.)
1) Recovery Service Provision
This is the most common way mental health services are held accountable: Are we providing the services we’re supposed to in sufficient amounts. In many parts of the system our payments are directly tied to service provision. It is also the weakest way to assess accountability. There’s no way of knowing if a service is being provided well or not, effectively or not, compassionately or not, etc. All we know is that, at least on paper, someone did something.
Recovery services can be described and counted as well as traditional psychiatric or rehabilitation services. I attached a list of recovery service areas that MHALA uses (attachment 2). These are included in our EHR alongside the medical service codes.
2) Recovery outcomes
It would be nice to know if we’re actually helping people recovery. We can track outcomes that are desirable whether they resulted from recovery or not, and we can track correlates of the recovery process.
California’s statewide AB2034 program that enrolled people who “deinstitutionalization failed” had four targeted outcomes: Psychiatric hospital days, incarceration days, homeless days, and employment days. The 70% reduction in hospitals, jails, and homelessness alongside a 400% increase in employment days were powerful outcomes for California’s legislature and Governor Schwartzneger. These four outcomes were specifically chosen to monitor the outcomes society had assigned to us and are relatively easy to track reliably. You could make a small set of similarly targeted outcomes, for example, reduced incidents of assault or other violence, increased incidence of competency restoration at hearings, employment earnings within the hospital, increase in board approved discharges to lower levels of community care, etc.
MHALA didn’t feel that the variables on our four stage map of recovery (hope, empowerment, self- responsibility, and meaningful roles) would be reasonably measurable to track recovery although they successfully captured subjective experiences of recovery. We created a tool that is uses staff ratings to track individual’s progress through recovery using three correlates of recovery – risk, engagement with mental health services, and skills and supports. This link has the eight point Milestones of Recovery Scale (MORS) and describes its development, validation, and use: http://mhavillage.squarespace.com/storage/84AGuidetotheMORS.pdf.
You could create a similar tool using the three most crucial outcome dimensions for your program – safety, freedom, and self-responsibility to define stages you could track people through; for example
stages like extreme danger, high external restriction, low internal control and self responsibility. Remember that the map shouldn’t be linear and should include forward and backward movements to realistically map recovery.
3) Recovery culture
On the face of it, culture is the most difficult thing to measure. MHALA has developed a tool for adult community based mental health programs that begins with seven core valued dimensions of a recovery culture and then describes concrete indicators of whether the program is doing nothing, exploring, emerging, maturing, or excelling in each area. This link http://mhavillage.squarespace.com/storage/87ARecoveryCultureProgressReport.pdf has the Recovery Culture Progress Report and a discussion of its rationale, development and usage. Note how each domain flows from a value statement. You could develop a tool like this for your own program.
Conclusion:
The same friend of mine I began with said that for hope to be useful it has to include three elements: 1) A vision of where you’re aspiring to get to that is clear and specific enough to become believable (not that you ever get to exactly where you imagined or hoped for), 2) A commitment to take a few concrete steps that lead towards your vision (and see what happens), and 3) Enough passion and understanding of why this vision is important enough to you that you’re resilient enough to make it through the inevitable blockades and setbacks.
I think you have enough useful hope to achieve recovery transformation at OSH. Thank you for including me in your journey.
WE BELIEVE…
MHAVillageGuidingPrinciples and the Stages of Recovery
- Hope makes recovery possible; it facilitates healing of the mind, body and spirit.
- Welcoming people includes creating a culture of acceptance with easily accessible integrated supports and services.
- Focusing on the whole person includes their strengths and weakness, abilities and barriers, wounds and gifts.
- Each person creates their path and determines the pace of their recovery.
- The recovery process is a collaborative journey in support of individuals pursuing their life goals.
- Relationships are developed through mutual respect and reciprocity, including openness to genuine emotional connections.
- A solid foundation for recovery is built by helping people to honestly and responsibly deal with their mental illness, substance abuse and emotional difficulties.
- People thrive, grow and gain the courage to seek change in respectful environments that promote self responsibility.
- The practical work of recovery takes place in the community.
- Each person has the right to fair and just treatment in their community ensured through advocacy and social responsibility.
- Everyone deserves the opportunity to have a place to call home.
- Promoting natural supports, having fun and a sense of belonging enhances quality of life.
- Employment and education are powerful means to help people build lives beyond their illness.
- Program success is based on achieving quality of life and recovery outcomes.
Recovery Based Service Categories and Vignettes
1) Welcoming / engagement – connecting the member with staff, program and peers, relationship building, demonstrating our “usefulness” to the member, engaging in collaborative goal setting, shared decision making, connecting with the member through self-disclosure
I asked Ann to bring in the drawings she’d made with the art supplies her mother had sent to the Board and Care, admired them, and made a couple copies to put on the wall. I also showed them to other members and staff who were sitting around the team area, introducing Ann as a “real artist”.
2) Crisis interventions / Responding to basic safety needs and community expulsion threats – accessing, collaborating with and/or diverting from hospitals and jails, advocating with the legal system to prevent incarceration, locating, placing in and/or paying for emergency shelter to prevent homelessness, , safety interventions – medical, substance abuse harm reduction and prevention, responding to threats of dangerousness, suicidality, and impending harm (e.g., domestic violence)
Donna wandered into the team area looking quite confused. She didn’t respond to anything I said, just staring at me. Yesterday she had been coherently calling checking her status on the waiting list for a rehab program, so it seemed likely she was high or coming down. We tried to get her to take some medication, but she wouldn’t. We watched over her and gave her a ride home where they know she gets like this a lot and can take care of her.
3) Assessments – assessing goals and needs, understanding their view of themselves, mental health status assessment, Quality of Life assessment, co-occurring conditions (e.g., medical, substance abuse, developmental disability), “eligibility” determinations (voc rehab, disabled students, SSI, bus passes), fitness determinations (legal competence, child custody and driver’s license)
Mike says he wants to get a job, but he seems far too disorganized and our employment staff is hesitant to work with him. We decide to give him a “we pay” job using client support funds to put together new charts and shred paper for us for one hour a day to see if he can show up and if he does, how he’s able to function at those tasks, and if he follows directions. The information gathered can also be used as part of his SSI disability report.
4) Building and maintaining the safety net / “protective factors” – assisting in obtaining benefits and entitlements, connecting to poverty services (e.g., COA food bank, multi-service center), charity (e.g., bus tokens, food, clothes, toiletries), safe and secure housing, family connections, assisting in obtaining basic documentation (e.g., ID, birth certificate), connecting to basic social
services (DPSS, SSA), connecting to cultural connections, (Native American services, UCC), connecting to spiritual strength and security (faith community)
Anna has been staying with a variety of men she finds, but they all end up taking her money and short lived. She seems always surprised when they pressure her for sex. We make a deal with Ann that if she contributes $150 per month out of her GR check, we’ll give her a hotel voucher worth $650 to have a safe place to stay for the month, but she can’t have any one stay in her room with her.
5) Motivating / Engaging in growth oriented activities – engaging in motivational interviewing, outreaching to isolated members, exposure to opportunities e.g., plays, sports, dances, hobbies, job fairs, schools), exploration of possibilities for the future, career exploration, core gift activities, goal visualizing, peer bridging
Carl hangs out at the sober living all day long, using pot and not following up with anything. He says he doesn’t have any money to do anything. I offer to take him out to lunch with a small group of members and on the way intentionally take him by one of the other member’s apartment starting a conversation about what it would take for him to get an apartment of his own too.
6) Treating mental illnesses and substance abuse disorders to reduce barriers – helping members to gain control over their mental illness, helping members to identify and control their symptoms (e.g., WRAP), 12-step step work, medication services, providing psychotherapy, building emotional coping skills (e.g., CBT, coping with past traumas, anger management, relationship skills), building wellness skills (e.g., meditation, eating and sleeping routines, yoga), treatment of acute symptoms and relapses
Renee is struggling with panic attacks and flashbacks of being raped and is overtaking the Klonipin she’s been prescribed combining it with alcohol. I teach her several anxiety reducing techniques including a “butterfly hug” to use during flashbacks, relaxation imagery for when she’s not quite as anxious, and to carry around a small tin of coffee grounds in her pocket that immediately calm her by reminding her of her mother when she was a child.
7) Treating physical illnesses – providing basic wound care, monitoring and treating chronic physical illnesses (e.g., diabetes, hypertension, chronic pain), medication management for physical illness medications, seizure response, physical illness education (e.g., diabetes, hepatitis), smoking cessation, promoting physical wellness (e.g., exercise and nutrition)
Dennis fell in the bathroom at the Village and said he was “knocked out” for a second. I called a nurse to check his vital signs and make sure he didn’t have any neurological signs that would indicate we should take him to an Emergency Room.
8) Providing and building support – connecting to Village resources (e.g., job development, educational) and community resources ( Jewish Community Center, Gay and Lesbian Center, primary care provider, 12-step support groups, warm lines), connecting to social services (e.g., In Home Supportive Services, Family Preservation), participating together in community
activities and opportunities (“giving moral support”), helping families to support members (e.g., family education, consultation, problem solving), providing help directly (e.g., “doing it for them,” adding structure to their lives, making decisions for them, ”caretaking”)
Martin needed to get help to move his stuff from his hotel room into a permanent apartment. He couldn’t get any friends or family to help him and he didn’t have $15 to pay day labor to do it with him. Since there wasn’t that much stuff, I drove my own car over and helped him put his stuff in my trunk and then helped him unload it into the apartment.
9) Rehabilitation / Skill building – teaching, job coaching, supported models (employment, education, housing), in-vivo teaching, providing work experience, teaching self-help skills (e.g., budgeting, shopping, laundry, hygiene, medication management), helping the member to build and practice meaningful roles
Kenny’s shower head broke off in his apartment. His girlfriend who lives with him demanded that he do something about it and threw it at him. He brought it in and put it on my desk demanding that I do something about it. First I coached him through the process of calling his manger with him on the phone talking but that got nowhere. Then we got in my car and I coached him through the process of actually getting a replacement part at the hardware store. Once again, he did the talking while I stood by his side giving him hints. He screwed the shower head back on himself. He wrote a letter to the manager, enclosing a copy of the bill, to get the money back sitting at my desk going over it step by step.
10) Building personal growth and responsibility – Helping members understand and move through normal stages of life (e.g., prolonged adolescence, first parenting, mid-life crisis, empty nest syndrome), building self- responsibility (learning cause and effect, not blaming others), building self- efficacy (building the ability to positively impact one’s life), empowering members
Andy was offered a catering job with the Village Deli on a Saturday for four hours, but that was also the day his case worker was taking some members on an outing to Universal Studios. Andy was torn between fun and responsibilities. While another immature member urged him to go to Universal Studios with them and just have fun, I helped them both see how cancelling out on his boss at the last minute would make him a less responsible employee and that fun has to scheduled around work.
11) Community integration – developing and facilitating members’ connections beyond mental health and social services (Taking a member to a Mommy and Me group, helping a member to join a bowling league, creating a calendar of low-cost community events), helping member to discover niches, roles, and opportunities in the community, promoting being a good neighbor and citizen, helping member to invest in and give to community in positive ways, helping the member to learn to give to others
Francis had been raised Catholic, but hadn’t been back to Church in many years while she’d been on the streets and using drugs and prostituting. Now she was clean, but felt too ashamed to return to
Church. I connected her up with another staff member who goes to Catholic Church regularly and he agreed to go with her and just sit in the back together during services to see how it felt.
12) Community development – making the community a better place for people with mental illnesses, increasing tolerance and acceptance of mental illness, reducing segregation, reducing stigma, developing welcoming hearts in the community, building connections with other community social causes
The East Village Association arranged for a community clean-up day. A group of members and staff came in together as a Village team to help this neighborhood effort.
13) Promoting self reliance, separation from services, and graduation – building financial independence (getting off SSI and Section 8), obtaining private insurance, preparing for graduation, facilitating relationship changes with staff, finding and providing opportunities to give back to others still struggling, developing self-advocacy skills, developing friendship skills
When Kathy called asking for my advice in her problem with her boyfriend, instead of giving her advice, I helped her explore who else she had in her life whose advice she could rely on, so she wouldn’t need me anymore.